Taenia solium; Pork tape wormK
- Taenia solium commonly known as the pork tapeworm or the armed tapeworm.
- It is a flat-ribbon like tape worms that causes intestinal taeniasis.
- Adult worms are rarely pathogenic but the encysted larval stage (cysticercus cellulosae) of the worm caused a serious disease in human called Cysticercosis.
Habitat:
- The adult worm inhabits the small intestine (upper jejunum) of human.
Morphology:
Adult worm:
- Adult Taenia solium is a flattened ribbon like tapeworm that is white in color.
- The adult worm measures about 2-3 meters in length.
- The body of parasite can be divided into 3 parts:- Head (Scolex), neck and body (strobila)
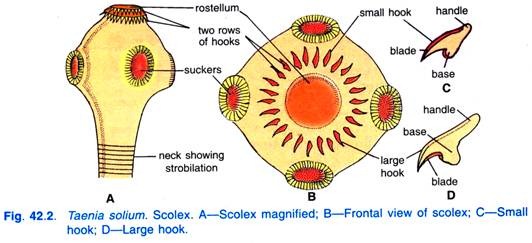
i. Scolex (Head):
- It measures 1 mm in diameter, about the size of a pin head.
- It is globular in shape and has 4 circular suckers.
- The head is provided with a rostellum armed with a double row of alternating large and small hooklets (130-180mm long).
- The presence of hooklets gave its name armed tape worm.
ii. Neck:
- The neck is short measuring 5-10 mm in length.
iii. Body (Strobila):
- The body or Strobila consists of segments or proglottids.
- The total number of proglottids are about 800-900.
- The proglottids may be immature, mature or gravid.
- The gravid segment measures 12 X 6 mm in diameter and looks grayish-black and transparent when fully developed.
- The worm is hermaphrodite and each segment containing both male and female reproductive organs.
- The common genital pore is marginal, thick-lipped and is situated near the middle of each segment alternating between the right and left side.
- Testes consists of 150-200 follicles.
- An ovary is two in number which has a third (accessory lobe).
- The ovary is situated in the posterior side of the segment.
- The gravid consists of a median longitudinal stem of uterus having 7-13 branches on each side of the segment.
- Uterus is completely filled with eggs and each gravid consist nearly 30,000-50,000 eggs.
- The vaginal opening is not guarded by a muscular sphincter.
- The gravid segment are expelled passively, in chains of 5 to 6 at a time and not singly.
2. Eggs:
- Eggs are similar to those of Taenia saginata.
- Each egg is round, brown in color, measures 40-50 µm in diameter
- Each egg consists of two shells.
- The outer shell is thin, transparent and represents the remnant of yolk mass.
- The inner shell, also known as embryophore is brown, thick walled and radially striated. It encloses the embryo.
- The embryo measures 14-20 µm in diameter with hooklets.
- Eggs do not float in saturated solution of common salt (NaCl).
- Eggs are infective to pigs as well as to humans.
3. Cysticercus cellulosae larvae
- Larvae is cysticercus cellulosae and is the Infective form of parasite.
- It is also known as Taenia cyst.
- The larval form develops in the muscle of pigs as well as various organs of the human.
- A mature cyst is an opalescent ellipsoidal body and measures 8-10 mm width by 15mm in length. It has a fluid filled milky white bladder like structure.
- The long axis of cyst lies parallel with the muscle fiber. The cyst is separated from the host tissue by a thin collagenous capsule. There is a dense milk white spot at the side, where the scolex with its hooks and suckers remain invaginated.
- The cavity of cyst is fill with a clear fluid rich in albumin and salts.
- The larvae can live for about 8 months in muscles of pig and can only develop into adults when ingested by man.
Life cycle of Taenia solium:
- The life cycle is completed in two hosts.
- Definitive host: Human
- Intermediate Hosts: Pig, occasionally human.
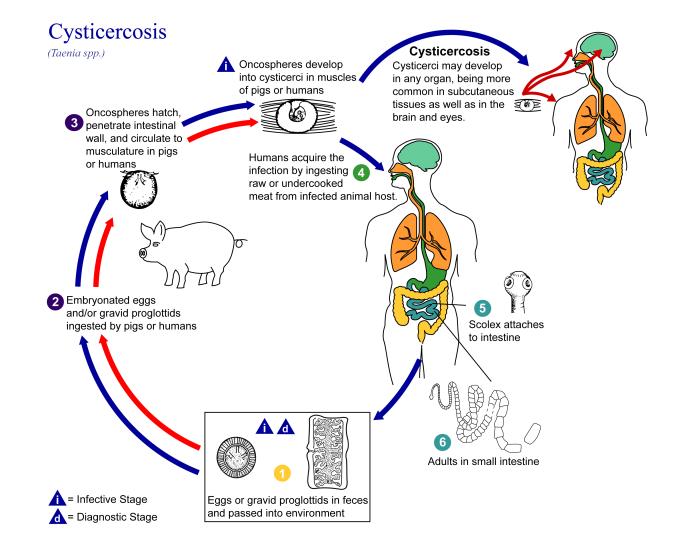
- Humans acquire infection by ingestion of inadequately or improperly cooked pork infected with cysticerci.
- Inside the alimentary canal of man the scolex on coming incontact with bile exvaginates and anchor to the gut wall with its hooks and suckers.
- The larvae develops into an adult worm by gradual strobilisation.
- The worm grows to sexual maturity in 2-3 months and start producing eggs which are then passes in the faeces along with the gravid segments.
- The pig gets infection by ingestion of eggs or gravid proglottids passed in human faeces.
- In the intestine of pig, the oncospheres hatch out of eggs.
- They attach to the intestinal mucosa by hooks, penetrate the gut-wall and gain entrance into the portal vessels or mesenteric lymphatic, finally reaching the systematic circulation.
- Usually they travel via the portal vein and successively reach the liver, right side of heart, lungs, left side of heart, brain or other tissue with high blood flow.
- The naked onchospheres are filtered out from the circulating blood into the muscular tissue where they ultimately settle down and undergo further development.
- They lose their hooklets, enlarge, and develops into a fluid-filled cyst within a period of 9-10 weeks.
- They remain viable for up to 8 weeks in muscle of pig during which they remain infective for human.
- The new host gets infection by ingestion of the infected meat of pig and the cycle is repeated.
- Occasionally humans get infection by eating food or drinking water contaminated with eggs.
- On ingestion, the onchospheres are released from the eggs in the intestine. These larva invade the intestinal mucosa and are then carried by the circulation to different tissue where they develops into cysts.
- In human most cysts are produced in the CNS, skeletal muscles, eye and subcutaneous tissue giving rise to a condition called cysticercosis.
Mode of transmission:
- Ingestion of uncooked pork infected with tape worm
- Ingestion of food and water contaminated by the eggs present in the infective faeces of a Taenia carrier.
- Endogenous auto infection: Anus-hand-mouth transfer of eggs by contaminated hands of person with poor personal hygiene.
- Autoinfection: Reverse peristalsis in which eggs produced by T. solium are thrown back to the duodenum, where they hatch and cause tissue infection
Pathogenesis of Taenia solium:
- Both adult worm and cyst are
pathogenic.
The adult worms are less pathogenic. They occasionally cause mild irritation or inflammation of the intestinal mucosa by their armed scolex. - The cyst, (Cysticercus cellulosae) are more pathogenic. They cause a serious disease cysticercosis in human, mostly cyst are produced in the skin, skeletal muscles, eye and CNS.
- The cyst can remain viable for few years.
- In the brain the cyst survives by overcoming the host defenses. It secretes the prostaglandins and other substances that inhibit activation of the complement and production of cytokines. This result in minimal host inflammation around the live cysticercus. The live cyst is surrounded by a local minimal cellular reaction that consists of few eosinophiles and macrophages.
- The dead cyst is surrounded by a dense infiltration that consists entire spectrum of inflammatory cells, including leucocytes and multinucleated giant macrophages, inflammatory cells and less frequently foreign body giant cells. Outside this area a zone of fibrosis and chronic inflammatory infiltration are present.
Clinical diseases caused by Taenia solium infection
1. Intestinal Taeniasis:
- Mostly the infection is asymptomatic.
- In symptomatic cases, the clinical symptoms are nonspecific and mild and includes- nausea, abdominal discomfort, hunger pain, loss of weight, chronic indigestion etc.
- Less frequently nausea, vomiting, headache and diarrhea are present in few cases.
2. Cysticercosis:
- Cysticercosis is the infection with the larval stage of the parasite.
- Human beings acquire infection through faccal oral contamination with T. solium eggs from tapeworm carriers or by auto infection.
- Clinical manifestation depend on the affected organ; neurocysticercosis and ophthalmic cysticercosis are associated with substantial morbidity.
i. Extraneural cysticercosis:
- Subcutaneous cysticercosis present as small, movable, painless modules that are commonly noticed in the arms or chest.
- After a few months or even years, the modules become swollen, tender and inflamed and then they gradually disappears.
- Muscular cysticercosis is a causal finding, appearing as dot shaped or ellipsoidal calcifications.
- In rare cases, very massive parasite burdens enlarge the patient’s limbs (muscular pseudohypertrophy).
- The heart is another occasional location, infected in about 5% of patient’s cardiac cysticercosis is asymptomatic.
ii. Ophthalmic cysticercosis:
- This condition is present in 20% of cases.
- Most cysts are found in the vitreous, subretinal space and conjunctiva.
- The condition may present as iritis, ureitis and palpebral conjunctivitis.
- The cyst in subconjunctival or subretinal sites may present as slowly growing nodules confusing with tumors.
- Occasionally, subretinal eye cyst may lead to blindness due to detachment of retina.
iii. Neurocysticercosis:
- The parasite commonly infects the CNS, causing neurocysticercosis as a clinical disorder.
- After entering the CNS, cysticerci are visible and elicit few inflammatory changes in the surrounding tissue.
- Cysticerci cause symptoms because of mass effect or by blocking the circulation of cerebrospinal fluid, most symptoms are the direct result of the inflammatory process that accompanies cyst degeneration.
- Symptoms and signs are varied and nonspecific.
- Epileptic seizures are the commonest presentation and generally represent the primary or sole manifestation of the disease.
- Seizures occur in 50-80% of cases with parenchymal brain cysts or calcifications.
- The disease also present with intracranial hypertension, hydrocephalus or both in 20-30% of cases.
- The syndrome is related to the location of parasites in the cerebral ventricles or basal cisterns blocking circulation of CSF and is caused by several different mechanisms- the presence of the parasite itself, ependymal inflammation or residual fibrosis.
- Occasionally a cyst grows larger than the usual and acts in the same way as a tumor mass (giant cyst).
- These giant cysts compress adjacent cerebral structures, causing localized deficits and intracranial hypertension. Motor deficits can also arise because of oedema secondary to cyst degeneration or as a result of stroke complicating the infection.
- In children and teenagers, an acute encephalitic presentation can happen, more likely in female than male. Massive non encephalitic forms also occur.
- Compromise of the spine occurs in adult 1% cases, presenting with compressive manifestation.
Laboratory Diagnosis of Taenia solium:
Specimen:
- Faeces, muscle tissue, blood, csf
1. Macroscopic examination:
- A naked examination of the specimen can be made for segment or proglottids.
- The whitish segment can easily be recognized against the dark yellow mass of the faeces.
2. Stool Microscopy:
- Demonstration of eggs and less frequently proglottids and scolex in faeces is used as tool for diagnosis.
- Eggs:
- Eggs are demonstrated by a thick faecal smear examination.
- The eggs shed irregularly, so 2-3 stool sample should be collected.
- Eggs can be seen in perianal area and can be detected by cellophane swab.
- Since eggs of T. soluim and T. saginata are similar, species diagnosis can be made by Acid-fast staining. Eggs of T. soluim are non-acid fast whereas T. saginata is acid fast.
- Proglottids:
- The gravid proglottids are found in faeces or recovered from the under clothings.
- They are washed in clean water and placed between two sides.
- The sides are held by adhesive tape at each end and are examined by hand less for lateral branches.
- Demonstration can be facilitated by staining them with india ink, injected through the genital pores.
- Observation:
- Taenia soluim: 7-12 lateral branches on each side of utetine stem
- T. saginata: 10-20 lateral branches on each side of utenine stem.
- Scolex:
- T. soluim – bears a row of hooks
- T. saginata- lacks hooks.
- The scolex is not always recovered following the treatment and the method is hazardous.
3. Antigen detection:
- This is a very useful for screening the cases of intestinal taeniasis.
- Antigens capture ELISA polyclonal antisera raised against Taenia is employed to detect antigen in faeces.
4. Serodiagnosis:
- Serological tests are employed to detect anti-cysticercus antibodies in serum or CSF.
- ELISA (sensitivity 75%, specificity 85%). Antigen can be detected by ELISA using specific monoclonal antibodies.
- Enzyme-linked immunoelectro transfer blot (EIIB). Sensitivity 90 % specificity 50-70%.
- Detection of antigens in serum or CSF indicates recent or viable infection.
5. Histopathological diagnosis
- Diagnosis of Neurocycticercosis (NCC) is made by demonstrating cysticerci in the biopsy tissue obtained from brain during post mortem.
- Skeletal cysticercosis can be diagnosed by histological examination of biopsy.
6. Imaging method:
- X-ray of the soft tissue in arm and thigh, chest and neck may show dead, calcified or elongated cysts.
- X-ray of the skull may reveal cerebral calcification and intracranial lesions in the neurocysticercosis.
- CT scan is best method for detecting dead, calcified and multiple cysts is pathognomonic of neurocysticercosis.
- MRI shows a mural nodule within the cyst which is pathognomonic for NCC.
7. Other test:
- CSF protein level are elevated in neurocycticercosis.
- CSF may show lymphocytosis- Mononuclear pleocytosis is frequent
- Glucose levels may be mildly to moderate low.
- Cell counts rarely exceed 300/mm3
- Eosinophils in the CSF are common but nonspecific binding
Treatment of tape worm infection:
i. Praziquantel– drug of choice.
- Dose- oral.
- 50 mg/kg body weight
- 3 divided doses for 15 days.
ii. Niclosamide:
iii. Albendazole:
- A dose of 400 mg twice daily for 30 days.
iv. Surgery:
- For cysticercosis of ocular, ventricular and spinal cord.
Prevention and control of taeniasis:
- Avoidance of eating raw or insufficiently cooked pork
- Inspection of pork for cysticerci.
- Proper sanitation facilities.
- Treatment of infected persons.
- Avoidance of food contaminated with eggs of T. solium
Epidemiology and geographical distribution
- Taenia solium is found worldwide.
- It is most common in pork-eating countries, usually in low socio-economic and poor sanitation.
- 50 million people are infected worldwide.
- T. solium infections are endemic in central and South America, non- Islamic countries of South East Asia, South Africa especially among the Bantu communities.
- Eastern Europe and China areas of highest prevalence include Latin America and Africa.
